My Antidepressant Makes Me Tired — What Can I Do?
April 03, 2023
Content created for the Bezzy community and sponsored by our partners. Learn More
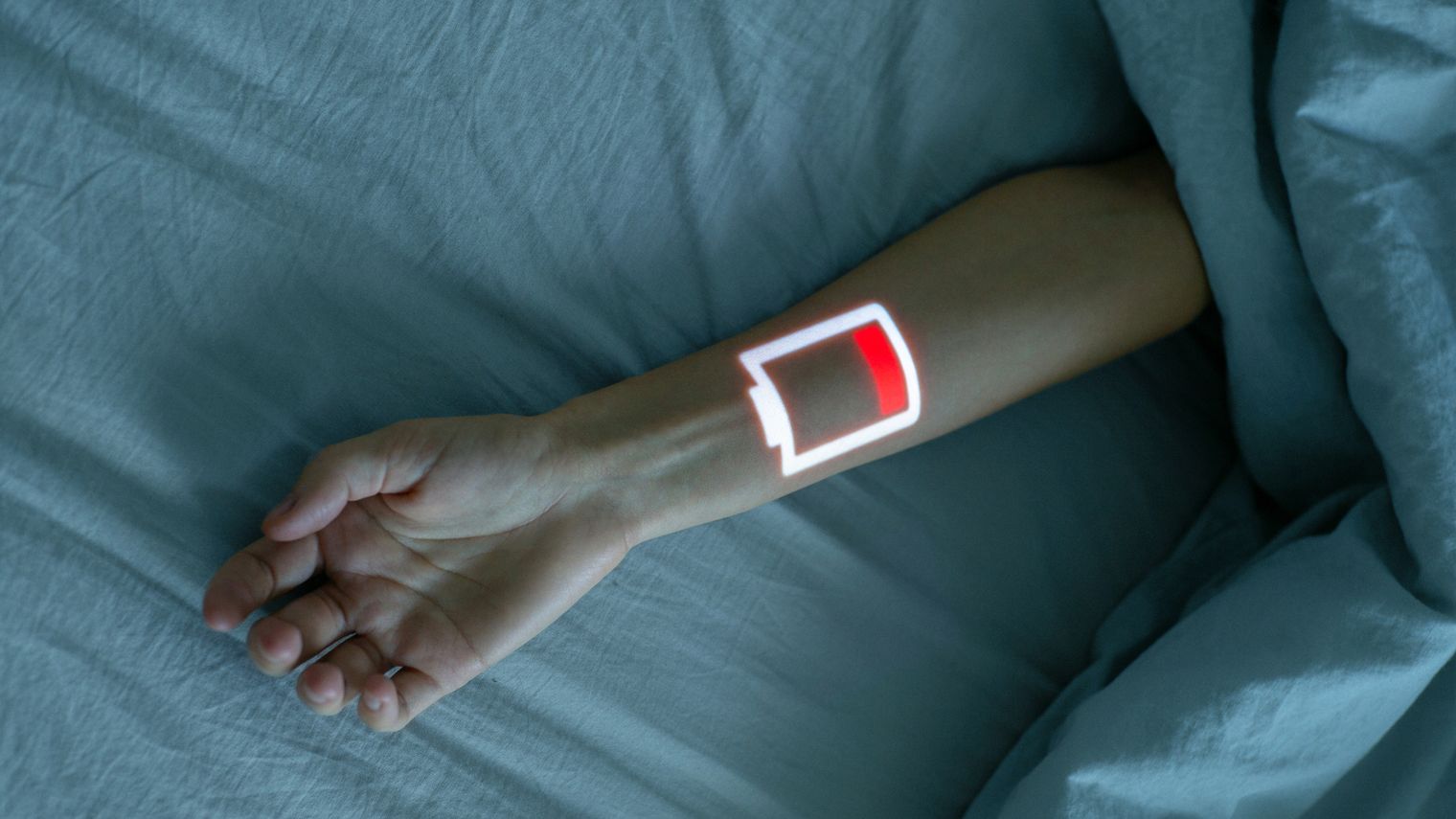
Photography by Duet Postscriptum/Stocksy United
Here’s a breakdown on why your medication might be making you sleepy, some energizing options, and things to consider when finding the best antidepressant for you.
Tiredness caused by antidepressants is a common side effect and can be concerning if it’s a regular occurrence. For many, it’s also counterproductive, especially if you already experience depression exhaustion. More than 90% of people with depression experience fatigue. Who wants to feel twice as tired due to the side effects? Well, no one!
Selective serotonin reuptake inhibitors (SSRIs), norepinephrine and dopamine reuptake inhibitors (NDRIs), Tricyclic antidepressants (TCAs), Monoamine oxidase inhibitors (MAOIs), and serotonin-norepinephrine reuptake inhibitors (SNRIs) are some of the common classes of antidepressants.
I’m sure you want to know which ones make you tired. I’ll discuss that below, including ways to overcome fatigue, why these medications are leaving you tired in the first place, some of the energizing antidepressants, and things to consider when figuring out the best antidepressant for you.


Antidepressants that cause fatigue
Doctors often start the course of treatment with an SSRI, which helps your brain produce enough serotonin to function properly. SNRIs are prescribed when your brain needs higher levels of serotonin than usual. This is why they’re called dual reuptake inhibitors — they inhibit reuptake or reabsorption of serotonin and norepinephrine. While some of them can cause some fatigue, not all of them do.
If you’re taking a TCA, you might experience extreme fatigue. This medication can be used for reducing pain and boosting sleep quality, so feeling more tiredness as a result is not unusual.
TCAs can be further broken down into secondary amine TCAs and tertiary amine TCAs. Secondary amine TCAs, like desipramine and nortriptylin, have higher norepinephrine reuptake inhibition than tertiary amine TCAs, like amitriptyline or doxepin. This means that secondary amine TCAs typically cause less sleepiness, although they can still cause it. This is also why amitriptyline and doxepin are sometimes used as insomnia treatments.
This older class of antidepressants tends to have more severe side effects on individuals. If you’re prescribed Elavil, Asendin, Sinequan, Anafranil, or Surmontil and experience fatigue plus dry mouth, confusion, bladder issues, or a racing heart, you may want to talk about this with your doctor.
MAOIs can also induce intense feelings of sleepiness. Basically, every MAOI is known to cause fatigue — Nardil, Parnate, Emsam, and Marplan. MAOIs and TCAs aren’t usually the first choice for treatment, because they do have more severe side effects, but for various reasons, your doctor might think they’re right for you. In this case, you might be more likely to experience noticeable fatigue.
Additionally, some antidepressants are actually used to promote sleep, such as trazodone and mirtazapine. These are considered the most sedating antidepressants, so you might want to avoid these if your goal is to prevent fatigue.
Why do antidepressants cause fatigue anyway?
Antidepressants influence various neurotransmitters in the brain, namely histamine, acetylcholine, norepinephrine, and serotonin. While these chemicals have many roles in the body, they all play a part in the sleep or wake cycle. So, changing the amounts of these neurotransmitters in your brain can also leave you feeling more tired or awake than usual.
Another fact you should be aware of is that you’re more likely to experience fatigue in the initial stages of antidepressant treatment. The tiredness sometimes lessens as your body gets used to the medication. Giving your body some time and trying not to worry too much if you suddenly feel fatigued is the key. A mild form of drowsiness in the beginning isn’t worrisome.
If you’re looking for a more in-depth understanding of how each separate class of antidepressants affects sleep continuity and cycles, this article provides a useful chart.
Antidepressants that don’t make you tired
Newer classes of antidepressants come with lesser side effects. Antidepressants that are known to be best for energy include Prozac (fluoxetine), Zoloft (sertraline), and Wellbutrin (bupropion).
Wellbutrin is a fairly new type of antidepressant. Some very recent types of antidepressants don’t even fall into any of the conventional classifications. They’re generally referred to as atypical antidepressants.
These antidepressants primarily work by stimulating neurotransmitters — dopamine, serotonin, and norepinephrine. These neurotransmitters are typically scarce when we have depression. The availability of one or more of these neurotransmitters is increased by these antidepressants in various ways.
But there are various factors that determine what antidepressant is not going to make you tired other than the antidepressant itself. An open and honest discussion with your doctor throughout your journey can be very helpful when figuring this out.
It’s also important to keep in mind that energizing antidepressants can alleviate depression exhaustion but they won’t cure chronic fatigue syndrome.
Ways to combat the fatigue
- Improve your sleep hygiene: If you continue to feel fatigued after moving past your initial stage, try improving your sleep hygiene. Sleeping during the day can disrupt your bedtime routine, making you more prone to stay up late. This can make you feel sleepier during the day and the cycle continues. It’s important to find a routine that works best for you.
- Explore different dosing times: Ultimately, all antidepressants affect people differently. If your medication makes you sleepy, consider taking it at night. If it keeps you awake, try taking it in the morning. As always, consult with your doctor when making this decision.
- Take a cold shower: As unpleasant as this sounds, you might be surprised at the potential benefits. Taking cold showers have shown to help depression symptoms in various ways, and increasing energy is one of them.
- Talk with a therapist: While antidepressants can relieve many symptoms, they don’t always solve everything. And if they’re making you overly tired, psychotherapy might be the best medicine for long-term benefits. But the combination of both can be more effective for some than these stand-alone treatments.
- Find an energizing activity: Activities that light you up mentally are also a great option. Listening to some music, bird watching, taking a walk, watching short clips that make you laugh, painting, meditating, journaling, or soaking up some Vitamin D, are all potential sources of natural stimulation.
- Try mood-boosting food: Eating something that triggers dopamine is another option. Chocolates are my go-to to decrease general depression exhaustion. In winter, it’s hot chocolate, and during summertime sadness, it’s a chocolate shake for me.
- Consider the role of alcohol: Since both antidepressants and alcohol can cause drowsiness, taking them together might worsen that effect. It’s important to be honest with your doctor about your alcohol and other drug intake to make sure you aren’t experiencing any negative interaction effects.
- Explore other medications: Your solution might be as simple as switching your medicines. It depends on your situation, but it’s possible that you haven’t found the right treatment for yourself. In some cases, you might just need to reduce the dosage prescribed to find the balance between effectiveness and manageable side effects. But in either case, always discuss it with your doctors first.
What antidepressant is right for me?
There’s no straightforward answer to this, unfortunately. As said above, everything is on a case-by-case basis. With conditions pertaining to mental health, the process of finding the right course of treatment can sometimes be longer than expected.
Even if the antidepressant works for you initially, it’s possible that it will stop working or be less effective after a while, depending on how your brain responds to these drugs. Finding what antidepressant is right for you in the long term might require some trial and error.
Here are some important things you can consider while figuring this out:
- Health conditions: If you have other health conditions, whether physical or mental, antidepressants may or may not work how they’re supposed to. It’s important to consider the interaction between all your medications.
- Particular symptoms: You might want to prioritize overcoming/tackling certain symptoms over other ones. Prozac, Paxil, and Celexa all fall under the SSRI class, but it doesn’t mean that all are energizing or work with the same symptoms. While Prozac is more energizing, Paxil and Celexa have more sedating effects.
- Side effects: It’s important to notice the side effects you’re experiencing, how strongly you experience them, and what medication they’re associated with. It can be difficult to do, but increasing self-awareness regarding your response to different treatments can only help the process.
- Insurance coverage: Certain antidepressants aren’t covered by all insurance plans. It sucks when one can’t afford the antidepressants prescribed. So, it’s important to find out what brands and versions are covered by your insurance and if they’re going to be as effective.
- Pregnancy or breastfeeding: How safe your antidepressant is comes into play more here during breastfeeding and pregnancy. Experts say that it’s OK to get off your antidepressant if you have mild depression. For people who battle with suicidal thoughts, it’s advisable not to stop their course. You need to know the risks associated so you can decide what’s best for you and your baby.
The takeaway
There are many things to consider when finding the right medication for you. You might find that the medication that brings you the most relief also has negative side effects, like fatigue.
If that’s the case, there are ways to help manage tiredness. But remember, this is an individual journey and the best option is to talk with your doctor and mental health professionals to determine the best path forward.
About the author
This article was written by Vartika Puranik. Vartika wears many hats — journalist, social media expert, copywriter, content strategist, writer and tarot card reader. Her work has been published on Huffpost, Forbes, Insider Business, Women’s Health Magazine, Discover Magazine and more. You can check out her tarot channel here https://youtube.com/@tarotmates and connect with her here LinkedIn Twitter Instagram
Medically reviewed on April 03, 2023
6 Sources


Like the story? React, bookmark, or share below:
Have thoughts or suggestions about this article? Email us at article-feedback@bezzy.com.